- Thread Author
- #1
One of the most important aspects to monitor in people who use anabolic steroids is the hematological profile, especially the hematocrit (HCT), which represents the proportion of blood volume occupied by red blood cells (erythrocytes).
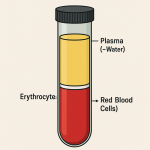
If you spin a tube of blood in a centrifuge, it separates into distinct layers:
Clinical threshold:
Centrifuged Blood and Its Layers -> see attachment
If you spin a tube of blood in a centrifuge, it separates into distinct layers:
- Plasma (≈55%): mostly water, electrolytes, proteins, hormones, and nutrients.
- Buffy coat (<1%): a thin layer containing white blood cells and platelets.
- Red blood cells (≈45%): packed erythrocytes, responsible for oxygen transport.
Reference Ranges and Gender Differences
- Normal hematocrit reference ranges vary slightly among laboratories (typically ~40–52% for men, ~36–46% for women).
- Women often have lower values due to blood loss during menstruation.
- In women who do not menstruate (e.g., due to menopause, hormonal suppression, or surgical intervention), it is normal to see higher hematocrit values closer to male ranges.
Why Elevated Hematocrit Is a Problem
Anabolic steroids (particularly testosterone and its derivatives) stimulate erythropoiesis (red blood cell production), often leading to secondary polycythemia.- When hematocrit rises significantly (>54–56%), blood viscosity increases.
- More viscous blood flows less easily and increases the risk of thrombotic events such as deep vein thrombosis, pulmonary embolism, stroke, or myocardial infarction.
- Studies have linked testosterone-induced erythrocytosis with a higher rate of cardiovascular events, especially in predisposed individuals.
Management: Therapeutic Phlebotomy
One of the most effective interventions is therapeutic phlebotomy (bloodletting).- A typical session involves the removal of 450–500 ml of blood.
- This should be done with isovolemic replacement: simultaneously infusing the same volume of saline into the opposite arm.
- Without replacement, the drop in blood pressure signals the body to compensate by producing more red cells, which may worsen the long-term problem.
- With saline replacement, blood pressure remains stable, and the erythropoietic stimulus is minimized.
Clinical threshold:
- Up to ~54% hematocrit is generally considered safe.
- ≥56% usually warrants phlebotomy to reduce viscosity and thrombotic risk.
Ferritin and Iron Status
- Low ferritin is always diagnostic of iron deficiency and should contraindicate phlebotomy, since further blood removal worsens the deficiency.
- High ferritin can reflect either real iron overload (storage excess) or an inflammatory response, so it must be interpreted in context (check CRP, transferrin saturation, etc.).
Key Takeaways
- Anabolic steroids frequently elevate hematocrit by stimulating red blood cell production.
- Elevated hematocrit increases viscosity and clotting risk; thresholds above 54–56% deserve medical attention.
- Therapeutic phlebotomy with isovolemic replacement is an effective strategy.
- Iron status (ferritin) must always be assessed before considering blood removal.